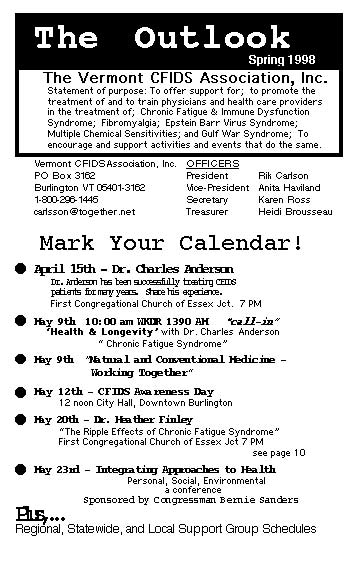
Newsletters: 1998
Contents:
- Editorial
- A Belated Christmas List... Mary Schweitzer
- CFIDS Research Funding is Endangered
- Sample Letter for CFIDS Research
- Vermonts Congressional Delegation
- Symptoms of Inner Peace - Faith L'Huereux
- Dr. Heather Finley - The Ripple Effects of Chronic Fatigue Syndrome
- Is There a Doctor in the House?
- First Do No Harm- An Editorial
- Mrs. Vermont Champions Chronic Fatigue Syndrome
- CDC Scraps Study of CFIDS in Youth
- What We Can Do
- Frustrations of a Physician by Patricia Salvato M.D.
Editorial
It was a difficult time when my physician told me
there was nothing more he could do. I had been driven to his office eight
weeks in a row and was devastatingly ill when he told me that.
"Go home and rest," he said, as if I had a choice.
That was the first wake-up call. On that day I learned that I had to become
the Doctor, and that to find recovery, I had to go beyond him and beyond
the insurance I had with CHP. I ached all over with flu, my brain was
mush and if I was up, I just stared at the floor. I was hardly ready to
begin medical school.
One year later I attended a support group meeting for people with Fibromyalgia
and learned that I wasn't alone. It was the first time I was with others
who were as sick as I was and I found some relief in that.
The Fibromyalgia group didn't specifically meet my needs and I learned
of the CFIDS group Jim Boyce had put together earlier. I picked up the
pieces and the rest is history.
It's been more than three years since that doctor told me there was no
known cure and nothing more he could do. In that time, because of the
people I've met and the wonderful health care providers who have taken
the time to share with us their successes, my health has improved. I'm
not out of the woods yet, but I can start to see through the trees and
I know that full recovery is possible. I understand the healing process.
I can't imagine where I'd be if I had stuck with my original doctor and
the confines of my health insurance.
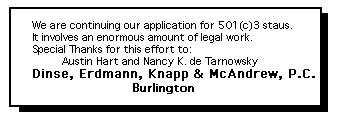
And that's why we're here. To go beyond the uneducated physicians and
antiquated health insurances. To learn from each other. To find the small
group of physicians and health care providers who know what this is and
who know how to heal. To restore our health. To be well again. That's
why we're here, and that's what we'll do. Happy Spring.
A Belated Christmas Wish...
What I want for Christmas...
My name is Mary Schweitzer. I have Chronic Fatigue Syndrome. It has been three years since I was last able to teach, publish, ski, hike,walk on the beach, drive a car, bake Christmas goodies, or join my husband and children in family activities.
What do I want for Christmas this year? Respect. I am not a liar, I am not a hypochondriac, and I am not a shirker.
Twice as many Americans have Chronic Fatigue Syndrome as have Multiple Schlerosis. Congress allocated only 13 million this year - about the same as they gave to study funny looking fish in the Potomac River. Starved for funds, research into the causes of the severe physical abnormalities in this disease creeps along slowly.
Temple researchers have shown that CFIDS victims are missing an important segment of RNA necessary for fighting viruses. This test remains unavailable to the public because of insufficient funding. A promising treatment has been held off the market for five years because of insufficient funds for testing: 80 desparate victims await the FDA's permission to join 20 others already paying $15,000 - 25,000 out-of-pocket for six months of IV infusions.
The disease attacks all races and income groups equally, yet 90% of those diagnosed are white and well-off. HMO's and clinics refuse to treat the disease; the NIH and NIAD publish diagnostic brochures, yet doctors receiving federal funds are free to insist they "don't believe in" Chronic Fatigue Syndrome.
Diagnosis is nearly meaningless in the face of an intractible society that equates disability insurance with con artists. Years of payments into FICA and private insurance plans prove meaningless when faced with beaurocrats determined to find a loophole with which to deny your claim. At best it takes one to four years to receive a penny from Social Security disability; private insurance companies with lawyers on retainer keep fighting until the claimant has no resources left with which to fight, and capitulates. Divorced housewives, students, those who left their jobs or agreed to work part-time before understanding how ill they were, face a future straight out of Dickens.
Rich or poor, the typical CFIDS victim will try to keep working until eventually they collapse, and those who collapse face a future of poverty no matter their original status in society. So why bother diagnosing those who are already poor?
What has happened to people in this country? Do we really think there are no invalids in our fantasy world? Or is America now closed to all except the vigorous and healthy?
What do we want for Christmas? Ignore the rediculous name the CDC has given us, and learn about this disease. Quit mocking us; quit treating us as guilty until proven innocent. In the richest nation in the world, invalids and their families should not have to suffer so.
Mary Schweitzer, 16 December 1997
CFIDS RESEARCH FUNDING IS ENDANGERED!
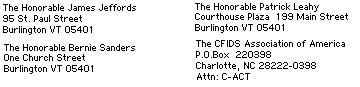
Elected officials rely on contact from their constituents to help them govern. Let's make sure that our members of Congress know that an effective federal response to CFIDS is important to us. Phone calls letters and faxes to Senators Leahy & Jeffords and Congressman Bernie Sanders is the best way to make sure our position is counted.
If you need additional convincing to write a few letters, think of this: Members of Congress have a different way of counting. Each letter they receive on an issue is tallied as 400 people who feel the same way but don't take the time to make their voices heard. They count each phone call as 150 people. It's easy to see why each letter or phone call can make a big difference!
SAMPLE LETTER FOR CFIDS RESEARCH
April 15, 1998
As one of your voting constitients, I urge you to support legislation that will raise the level of attention to Chronic Fatigue and Immune Dysfunction Syndrome (CFIDS) and increase the money spent on the study of CFIDS by our national public health agencies.
I along with more than 400,000 Americans have CFIDS which is also known as Chronic Fatigue Syndrome (CFS). Despite its name, CFIDS is a terribly debilitating and serious illness, with symptoms ranging from severe widespread pain to neurological impairments.
(This is a good place to tell your personal CFIDS story.)
On May 14, a group of CFIDS advocates will be in Washington to talk with legislators about CFIDS. Since I am to ill to come to Washington, I would appreciate if a member of your staff could set aside a few minutes to meet with them and learn more about CFIDS and its effects on people like me.
Please ensure that the federal government mounts an effective campaign to understand CFIDS so that progress in the understanding of CFIDS doesn't come to a halt.
Sincerely yours,
The Vermont Delegation:
The Honorable James Jeffords
95 St. Paul Street
Burlington VT 05401
1-802-658-6001
The Honorable Bernie Sanders
One Church Street
Burlington VT 05401
1-800-339-9834
The Honorable Patrick Leahy
Courthouse Plaza
199 Main Street
Burlington VT 05401
1-802-863-2525
Symptoms of Inner Peace by SASKIA DAVIS
submitted
by Faith L'Huereux:
Be on the lookout for symptoms
of inner peace. The hearts of a great many have already been exposed to
inner peace and it is possible that people everywhere could come down
with it in epidemic proportions. This could pose a serious threat to what
has, up to now, been a fairly stable condition of conflict in the world.
Some signs and symptoms of inner peace:
* A tendency to think and act spontaneously rather than on fears based
on past experiences.
* An unmistakable ability to enjoy each moment.
* A loss of interest in judging other people.
* A loss of interest in judging self.
* A loss of interest in interpreting the actions of others.
* A loss of interest in conflict.
* A loss of the ability to worry. (This is a very serious symptom.)
* Frequent, overwhelming episodes of appreciation.
* Contented feelings of connectedness with others and nature.
* Frequent attacks of smiling.
* An increasing tendency to let things happen rather than make the happen.
* An increased susceptibility to the love extended by others as well as
the uncontrollable urge to extend it.
WARNING:
If you have some or all of the above symptoms, please be advised that
your condition of inner peace may be so far advanced as to not be curable.
If you are exposed to anyone exhibiting any of these symptoms, remain
exposed only at your own risk.
SASKIA
DAVIS
Saskialucia@earthlink.net
(206) 364-7762
10640 Exeter Ave. N.E.
Seattle, Washington, 98125
Dr. Heather Finley, May 20th, 7:00 at the
First Congregational Church of Essex Junction
The Ripple Effects of Chronic Fatigue Syndrome
An informational and interactive discussion focusing on the experience of CFIDS in multiple aspects of life, including family relationships, work and productivity, the medical system, social activities, and personal identity
Dr. Finley is a doctoral level counseling psychologist specializing in behavorial medicine. Her clinical areas of focus include individual and group psychotherapy, addressing chronic pain, womens issues, mood disorders and substance abuse.
First Do No Harm
Do you know a good Doctor? Over and over, it's what we hear. And slowly over the past couple of years we've developed a small list of skilled and compassionate physicians who have knowledge and experience in dealing with CFIDS and Fibromyalgia and Chemical Sensitivities. And for that we are grateful. But the mainstream medical community is coming up empty. Desparately ill people are being sent home misdiagnosed and misunderstood. One reason we hear is that because there's no confirming test to clearly 'mark' this disease, (it's on its way), there's no reason to believe it exists at all, or another is, that there is no FDA approved cure, so there's 'nothing we can do'. Nothing. And people who clearly need guidance and understanding are sent off with confusion and disbelief and their families don't know what to do and their employers don't know what to do, and they don't know what to do and they try to force themselves to function more than their body allows and they worsen. And sick people get sicker and any proposed recovery time is profoundly extended.
And that's the dilemma. This is crazy. It's one thing to be sick but it's wholly another to be sent packing by those who've chosen to heal.
So here's what we do. The center page of this newsletter is a powerful letter from Dr. Patricia Salvato on her experiences treating CFIDS patients. That's right, treating, as in caring for, as in aiding the rocovery of, CFIDS patients. While there's no known cure, there are dozens of symptomatic remedies and understandings that can make a life that was once destroyed by this disease into a way of living that promotes the healing process and leads towards recovery. It can happen. Quite frankly it's the only way out. Read her letter, it's on page 7. Bring it to your doctor.
The back side of the letter is a physicians reference form. Ask him/her to fill it out and send it back to us. If your physicians want to learn more we can teach them. We have materials. There is an exceptional conference in October in Cambridge Massachusetts, (see following page), and we need local physicians to attend and bring this knowledge back to Vermont.
If we don't do this no one else will. We need to find out who the healing physicians are and where they are, and what insurances cover their services and list them for all to see and choose.
We need to do this now.
Let the healing begin.

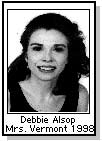
Mrs. Vermont Champions Chronic Fatigue Syndrome
In June, our very own Debbie Alsop was crowned Mrs. Vermont at a beauty pageant in Rutland, and with that she became the Official Representative of Vermont in the prestigious 1998 MRS. AMERICA PAGEANT. Debbie, who is no stranger to the debilitating restrictions of CFIDS has dedicated her reign to our group with the hopes that the attention she can bring to CFIDS in Vermont will enlighten the path to recovery. Her trip to Las Vegas to the Mrs. America Pageant was a challenge, but she found encouragement in the support she received from her husband Bob, support group members, and the other contestants.
Debbie Alsop was born in St. Albans, graduated from Castleton State College and is a registered nurse. Before CFIDS she worked full time and was a volunteer with Fairfax Rescue.
She tries to live within the boundaries of the disease although she admittedly has stretched them with this effort. She gets strength from the knowledge she has gained through the support group and in prayer. We extend our heartfelt congratulations to Debbie and look forward to the awareness of CFIDS that she will foster in the upcoming year. Thanks from us all.
CDC Shifts Funds: Scraps Study of CFIDS in Youth
CDC's (Centers for Disease Control) branch chief Dr. William C. Reeves, says CFS research funds are used to cover shortfalls and pay unrelated expenses in other programs and that the agency intentionally misrepresents CFS spending to congress and the public. Progress in a fundamental study of Chronic Fatigue Syndrome in children and adolescents was halted because agency officials did not approve funding. Study scientists were told that overspending in other programs contributed to the decision to block this study, which was to be the first of its kind. Congress first urged the CDC to begin investigating youth with CFIDS in 1996, and now, without immediate action, this study will be delayed until the year 2000.
The youth study is the latest casualty if fiscal misconduct at CDC involving CFS spending. In a compelling three page statement, Dr. Reeves reported end-of-fiscal-year juggling that switched CFS research funds into other programs. He told of a meeting in which a CDC official stated that he "always used CFS funds to make up for shortfalls elsewhere." The decision not to fiund the youth study appears to follow this established pattern.
Reeves letter is posted on The CFIDS Association of America's website at http://www.cfids.org/news/, along with a letter from Kim Kenney, Dr. Dedra Buchwald, and Dr. Anthony Komaroff to Secretary for Health Dr. Donna Shalala protesting the cancellation of the youth study.
What we can do!
Our immediate goal is launching a General Accounting Office (GAO) inquiry into CDC's CFS program. Rep. John Porter has expressed interest in asking for this audit. His support is crucial because, as chairman of the House committee in charge of health funding, his request will carry a great deal of weight with the GAO. Support from other members of Congress is critical in accelerating this probe. Please write to our Congressional Delegation and ask that they write a letter to Rep. Porter supporting his inquiry into misuse of federal CFIDS research funds. The addresses are below, and a sample letter is on page 11. Also please send a copy of your letters to the CFIDS Association of America so they can track response to this effort.
Sample Letter
Dear Senator [or Representative] (last name)
Rep. John Porter has expressed interest in requesting the general accounting
Office to launch an investigation into alleged misuse of chronic fatigue
and immune dysfunction syndrome (CFIDS) research funds at the U.S. Centers
for Disease Control and Prevention (CDC).
As a voter and taxpayer from [city] I am very concerned about this misuse of taxpayer dollars. As on of at least 500,000 Americans with CFIDS, I am angry that money that was intended and reported as having been used for research into the disease from which I suffer has been diverted into other programs. CDC researchers claim that they don't have enough money to do CFS research because they receive only a third of what is reported to Congress as directly supporting CFS research.
[ Include a paragraph about your experience with CFIDS.]
Please write to Rep. Porter and tell him that you and your constituents support a GAO investigation of this matter and appreciate his commitment to discovering the truth about CFS funding at CDC.
Sincerely yours,
cc: The CFIDS Association of America
Frustrations of a Physician Treating Chronic Fatigue Syndrome
c 1996 Patricia M. Salvato, MD
This year I enter my 11th year of practice. Some call me an HIV specialist while others call me a Chronic Fatigue Syndrome specialist. Although these two groups of patients make up a large majority of my practice, I also have a very active Internal Medicine practice including over 100 nursing home patients. I consider myself a specialist in Internal Medicine. Perhaps no other training would have prepared me more for my future as a practitioner in Chronic Fatigue Syndrome than my Internal Medicine training. The practice of medicine is an art which is far more than the application of scientific principles to a particular biological model. Its focus is on the patient whose welfare is the continuing purpose. That purpose of medicine is self-evident in theory, but more difficult to sustain under the pressures of medical practice. This is no more true than in the field of CFIDS which for years has been both ignored and ridiculed by a large part of the medical community.
I was asked to write about the frustration in treating patients with CFIDS. Many superficial hassles comes to mind - lists of endless symptoms; pages of questions without answers; disability letters and repeat disability letters and repeat disability letters; medical necessity letters to insurance companies; applications for disabled parking permits; letters to families, schools, employers, courts, attorneys and other doctors explaining the physical limitations of patients with CFIDS. As I think on a deeper level, however, the main frustration seems to center around my feelings in treating the disease rather than the increased work load of endless paperwork and extended office visits. Perhaps the thing that comes to mind the most is that as a physician I was taught that to be a 'good doctor' was to 'cure' disease. The patient comes to the doctor with a medical problem such as a sore throat, you give them an antibiotic, and two days later they are well. In my medical training, little time was devoted to managing the day-to-day care of a relapsing and remitting disease, where no cure was in sight and where patients did not get better over time but also did not die. Yes, I was exposed on many occasions to the dying cancer patient and in more recent years to the dying AIDS patient, but very rarely to the patient forced to live with a chronic debilitating disease that is poorly understood by the medical profession, family, the community, and even the patients themselves. In the first five to six years of dealing with CFIDS patients, I often left the office for the day feeling like a failure. Maybe one out of thirty patients actually would say they felt better. I didn't really get it that they didn't have to feel better for us to have a good physician/patient relationship. What I did learn was that the patients wanted to be listened to, so that their fear and concerns could be fully expressed and the burden shared. They wanted me to be interested in them as fellow human beings in a compassionate but non-judgmental fashion. They expected professional competence incorporating the best in medical science and technology. They wanted to be reasonably informed as to the probable cause of their concerns and what the future was likely to hold. They wanted riot to be abandoned. They did not expect to be cured, only I had expected to cure them. There is a certain mystery here, and it is an aspect of medicine that has been forgotten by too many physicians. Sir William Osler used to teach that if a physician made himself/herself available as a source of hope and strength to the patient, even with an incurable illness, without the use of medicine or fancy technology, these acts of professional skills alone could turn the tide. I believe these things even though I do not understand them.
Chronic Fatigue Syndrome has been the focus of increasing national and medical attention over the last decade. A growing number of research investigators are seeking to unravel the interrelationship of the psychologic, immunologic, neurologic and endocrinologic abnormalities associated with this debilitating disorder. Considerable misinformation still exists regarding the appropriate evaluation and management of the patient. CFIDS has lead to a necessary new paradigm in the doctor/patient relationship, one in which related information and knowledge have become recognized as critically important tools of healing. The nature of this disease and the fact that no single treatment provides a cure- brings doctor, patient, and loved ones into near constant discussion of a bewildering array of therapies. There is no FDA approved treatment for CFIDS. However, there are a variety of both symptomatic medication as well as holistic approaches which have empowered people living with CFIDS to take charge of their health. The physician must rely on his/her knowledge and judgement in assessing the risks versus benefits of treatment for each individual patient. One of the greatest lessons I have learned in treating CFIDS has been the realization that well-informed patients simple make better partners in health care, and, when knowledge is shared, everyone benefits; there is an unbelievable amount of healing in just the sharing of new knowledge.
Chronic Fatigue Syndrome presents a major public health problem for the 1990's, affecting more than a million people around the world. CFIDS can strike suddenly and linger for years, threatening personal relationships and careers. And devastating a persons life. Still, a large proportion of the medical community refuses to recognize the suffering it can cause. Patients with the disease cope not only with the illness itself but with the high medical bills, insufficient insurance coverage, and a tragic lack of emotional support often from physicians, caregivers, and even loved ones. Social Security disability payments are hard to obtain and the fear of their unknown future looms daily.
Another source of frustration in treating CFIDS patients has come from my relationships with my peer-physicians over the past 11 years.
The first 5-6 years were the most difficult, with the last five years adefinite trend toward at least receiving recognition of the disease by many physicians. I have found that the best way to 'educate' a disbelieving physician about the disease is to actually send them a CFIDS patient for evaluation of a specific problem, such as gastrointestinal, cardiac or neurologic. More often than not, the response that I get is, "you know, that patient is really sick." I am still amazed when they are so surprised. My own experiences with CFIDS have convinced me beyond doubt that it is an organic medical illness. I have seen an array of patients from all different walks of life, including housewives, blue-collar workers, athletes, physicians, nurses, educators, accountants and lawyers. In general, these people had been productive, on-the-go people, cut down in the prime of their lives.
This year has been the most rewarding in CFIDS, especially in view of the CDC's new role in the recognition of this disease and attempts at dispelling the popular belief that CFIDS is a benign, self-limited disease that affects only whites with high incomes. Dr. William reeves, head of the infectious diseases section of the Centers for Disease Control, has reported that only 12% of the patients with this disease ever fully recover. CDC officials have recently added CFIDS to the list of Priority 1 - New and Emerging Infectious Diseases [listing]. An NIH conference sponsored for physicians treating this disease was held this past year, the purpose of which was to identify outcome measures to be used in the evaluation of clinical trials. Based on rigorous discussion of outcome measures, clinical studies are now being initiated in this devastating disease.
Now more than ever, physicians and scientists are absorbed in scientific efforts to understand the etiology, epidemiology, and pathology of CFIDS, a complex, multisystem illness. For the physician or researcher willing to tackle this exasperating illness, the payoff is the opportunity to unravel an unsolvable medical mystery and thus preserve the passion of medicine.
I'd like to close by saying that my CFIDS patients have been a continued source of encouragement to me in my practice. I receive many letters and cards of appreciation from my patients. This past Christmas, I received a book from one of my CFIDS patients entitled When You Wish Upon A Star. The marker was placed in by a saying by O.S. Marden, which, in my mind, goes to the essence of being a physician treating this disease: "There is no medicine like hope, no incentive so great, and no tonic so powerful, as expectation of something tomorrow."
My expectation of something tomorrow is a better understanding of the cause of this debilitating disease and the possibility of a treatment capable of returning patients to their lives and their dignity.